🧠 Understanding Herniated Discs: Causes, Symptoms & Treatment Options (Including Massage and Microcurrent Therapy)
- Nicole Longwell

- 22 hours ago
- 5 min read

🧬 What Is a Herniated Disc?
A herniated disc (also called slipped or ruptured disc) occurs when the soft inner core of an intervertebral disc (nucleus pulposus) pushes through the tougher outer ring (annulus fibrosus). This can irritate nearby nerves and lead to pain, numbness, and weakness depending on where the herniation occurs.
Disc Bulge vs. Disc Herniation: What’s the Difference?
A disc bulge occurs when the outer layer of the disc extends beyond its normal boundary but remains intact, often affecting a broader area of the disc and commonly associated with age-related changes. A disc herniation, on the other hand, happens when the outer layer tears or weakens, allowing the inner disc material to push outward and potentially irritate nearby nerves. While both can cause pain or neurological symptoms, herniations are more likely to produce sharp, radiating pain, numbness, or weakness due to direct nerve involvement. Importantly, many disc bulges and herniations can be managed successfully with conservative care.
📊 Key Statistics You Should Know
Prevalence: Herniated discs affect roughly 1 – 3 % of adults in many populations and are most common between ages 30 – 50 years.
Most Common Levels: About 95 % of lumbar disc herniations occur at the L4–L5 or L5–S1 segments of the spine.
Lifetime Back Pain: Nearly 80 % of people will experience low back pain at some point, with herniated discs among the leading causes.
⚙️ Causes of Disc Herniation
Disc herniation usually develops from a combination of mechanical stress, age-related changes, and nervous system influences, rather than a single event. Common contributing factors include:
🧬 Degenerative Changes
As we age, intervertebral discs naturally lose hydration and elasticity. This reduces their ability to absorb shock and makes the outer disc fibers more vulnerable to small tears, allowing disc material to migrate outward over time.
🪑 Repetitive Strain & Prolonged Postures
Frequent bending, twisting, lifting, or long periods of sitting — especially with poor posture — increase pressure on spinal discs. Over time, repetitive micro-stress can weaken the disc structure and lead to bulging or herniation.
🏋️ Sudden Load or Improper Lifting
Lifting heavy objects without adequate core engagement or spinal support can sharply increase disc pressure. This is one of the more common triggers for acute disc herniation, especially in the lumbar spine.
🧠 Muscle Imbalances & Movement Patterns
Weak core stabilizers, tight hip flexors, or limited spinal mobility can shift stress onto specific disc segments. When muscles don’t distribute load efficiently, discs may compensate and become vulnerable to injury.
🚬 Lifestyle & Metabolic Factors
Smoking, poor circulation, and metabolic conditions such as diabetes can reduce blood flow and nutrient exchange to spinal discs, impairing tissue health and repair capacity.
🧬 Genetic Predisposition
Some individuals inherit disc structures that are more susceptible to degeneration or injury, making them more prone to herniation even with minimal stress.
🧠 Nervous System Stress & Guarding
Chronic stress and nervous system dysregulation can increase muscle tension and protective guarding around the spine. This constant tension may alter movement patterns and increase disc loading over time.
✨ Clinical Insight
Disc herniation is often the result of cumulative stress, not a single moment of injury. Addressing posture, movement habits, tissue health, and nervous system regulation can play an important role in both prevention and recovery.
📍 Symptoms — Based on Direction & Location of Herniation:
👉Cervical Herniation
Herniated Disc Level | Nerve Root Affected | Common Pain Pattern | Possible Symptoms |
C3–C4 | C4 | Neck and upper shoulder | Neck pain, shoulder tightness, limited neck motion, headaches |
C4–C5 | C5 | Shoulder and upper arm | Shoulder pain, deltoid weakness, difficulty lifting the arm |
C5–C6 | C6 (most common) | Neck → shoulder → outer arm → thumb | Arm pain, thumb numbness/tingling, weakened biceps, reduced grip strength |
C6–C7 | C7 | Neck → shoulder → back of arm → middle finger | Triceps weakness, tingling in middle finger, arm heaviness |
C7–T1 | C8 | Neck → inner arm → ring & little finger | Hand weakness, reduced fine motor control, numbness in ring/little finger |
🧠 How Direction of Herniation Matters in the Cervical Spine
Posterolateral herniations (most common) typically compress one nerve root, causing symptoms down one arm
Central herniations may affect the spinal cord and cause:
Bilateral arm symptoms
Coordination changes
Balance issues
Widespread weakness
Foraminal herniations specifically affect nerve roots exiting the spine and often worsen with head rotation or side-bending
👉 Thoracic (Mid-Back) Herniations
Thoracic herniations are less common but can be more difficult to diagnose.
Possible symptoms include:
Mid-back pain
Rib, chest, or abdominal pain
Sensations that mimic cardiac or gastrointestinal issues
Increased discomfort with rotation or deep breathing
👉Lumbar Herniation
Herniated Disc Level | Nerve Root Affected | Common Pain Pattern | Possible Symptoms |
L1–L2 | L1 | Groin, upper hip | Hip flexor weakness, groin pain, altered sensation in upper thigh |
L2–L3 | L2 | Upper thigh | Thigh pain, difficulty lifting the leg, reduced hip strength |
L3–L4 | L3 | Front of thigh, inner knee | Knee weakness, reduced sensation in thigh, difficulty climbing stairs |
L4–L5 | L4 (very common) | Low back → thigh → inner lower leg | Knee extension weakness, reduced patellar reflex, shin numbness |
L5–S1 | L5 / S1 (most common) | Buttock → back of leg → calf → foot | Sciatic pain, foot or ankle weakness, numbness in heel or outer foot |
🧠 How Direction of Herniation Matters in the Lumbar Spine
Posterolateral herniations (most common) compress a single nerve root and typically cause one-sided leg pain (sciatica)
Central herniations may affect multiple nerve roots and can lead to:
Bilateral leg symptoms
Increased weakness
Possible bowel or bladder changes (medical emergency)
Foraminal herniations irritate nerves exiting the spine and often worsen with:
Prolonged standing
Side bending
Lumbar extension
✨ Clinical & Wellness Insight for Lumbar Disc Herniations
Lumbar disc herniations often create protective muscle guarding, altered gait, and fascial tension throughout the hips and pelvis. Supportive therapies such as therapeutic massage, nervous system regulation, targeted movement, and microcurrent therapy may help reduce pain sensitivity and support functional recovery when used as part of a conservative care plan.
🧠 Treatment Options Explained - Non-Surgical
✔️ Conservative Treatment (First-Line)
Most people with herniated discs improve with non-surgical care over several weeks.
🩹 Rest & Activity Modification
Short periods of rest followed by gradual activity help reduce pain and promote healing.
💊 Medications
NSAIDs or muscle relaxants may ease inflammation and discomfort temporarily.
✋ Manual Care & Massage Therapy
Manual therapies and therapeutic massage are commonly used to reduce muscle tension, improve circulation, and support relaxation around the spinal region. While evidence quality varies, many patients report relief in tension and pain symptoms when manual treatment is part of an integrated plan.
Massage benefits may include:
Reduced soft-tissue guarding
Improved flexibility of surrounding muscles
Support for posture and movement habits
👉 Note: There’s limited high-quality clinical evidence specifically proving massage resolves disc herniation itself — but it can improve comfort and functional mobility as part of comprehensive care.
⚡ Microcurrent Therapy — A Complementary Option
Microcurrent therapy uses very low-level electrical currents (microamps) applied through the skin to support pain relief, reduce inflammation, and may enhance cellular function. This form of therapy is non-invasive and often used alongside other treatments to support recovery from musculoskeletal pain and inflammation.
Potential benefits reported include:
Reduced nerve-related pain and inflammation
Enhanced tissue healing and ATP production
Balanced cellular signaling and improved range of motion
While evidence specific to herniated discs remains emerging and clinical support varies, microcurrent can be a gentle, drug-free adjunct to standard care when used appropriately.
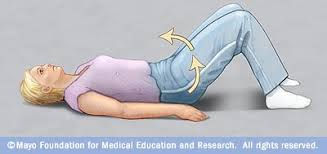
🚴 Exercise & Physical Therapy
Targeted physical therapy helps reinforce core muscles, improve posture, and reduce mechanical stress on discs. Exercise therapy has been shown to enhance pain scores and functional outcomes compared with no therapy.
🛠 Surgical Options
If conservative care (6–12+ weeks) doesn’t relieve pain or neurological symptoms worsen, procedures like microdiscectomy may be considered. Surgery removes a portion of the disc pressing on nerves and often improves leg pain significantly compared with persistent compression.
🧠 Final Thoughts
Herniated discs are common, especially in adults aged 30–50. Symptoms vary widely based on location and direction of herniation. Conservative care — including manual therapy, massage, therapeutic exercise, and complementary modalities like microcurrent — plays a central role for most people. Early diagnosis and a tailored treatment plan can significantly improve quality of life.



Comments